Dear Jeff Sessions: Here’s that science on marijuana and opioids you were asking for
Published: Mar 1, 2017, 7:38 am • Updated: Mar 1, 2017, 7:40 am
By Christopher Ingraham, The Washington Post
Speaking Tuesday morning before the National Association of Attorneys General, U.S. Attorney General Jeff Sessions expressed doubt that marijuana could help mitigate the opioid abuse epidemic.
“I see a line in The Washington Post today [Monday] that I remember from the ’80s,” Sessions said. “‘Marijuana is a cure for opiate abuse.’ Give me a break. This is the kind of argument that’s been made out there to just – almost a desperate attempt to defend the harmlessness of marijuana or even its benefits. I doubt that’s true. Maybe science will prove I’m wrong.”
The stakes are pretty high here. After all, opioids killed 33,000 people in 2015, up from around 8,000 in 1999. As the head of the Department of Justice, Attorney General Sessions oversees the Drug Enforcement Administration, which just last year reaffirmed its belief that marijuana has no medical value and hence should remain illegal (which makes it substantially more difficult for researchers to conduct studies).
Here’s a run-down of where the evidence on marijuana and opiates stands.
Marijuana is great at treating chronic pain.
This is the big finding, and the one from which all the others spring. Surveying the entire known universe of studies about the medical efficacies of cannabis, the National Academies of Science, Medicine and Engineering found “strong evidence” showing marijuana is effective at dealing with chronic pain in adults, relative to a placebo. The National Academies study is the most thorough review of the literature on marijuana to date, conducted by some of the nation’s leading substance use researchers.
Across numerous trials and experiments, the report found, people treated for pain with marijuana were “more likely to experience a significant reduction in pain symptoms” compared to a placebo or doing nothing at all.
This is huge news, considering the annual opiate overdose numbers cited above. Americans consume roughly 80 percent of the world’s opiate painkiller supply. The drugs are often prescribed for long-term treatment of chronic pain, a practice that the Centers for Disease Control and Prevention is now trying to discourage. Prescription painkillers and other opioids are highly addictive, and taking too much of them can easily kill you.
Marijuana is habit-forming too, but not nearly as much as opiate drugs like heroin. It also has no known lethal dose – you basically can’t consume large enough quantities of marijuana at a fast enough pace for overdose death to become a concern the way it is with say, OxyContin or fentanyl – or alcohol for that matter.
There’s been a lot of research done into this question in recent years. Here’s what it says:
States with medical marijuana laws see fewer opiate deaths.
According to a 2014 study in JAMA Internal Medicine, states with medical marijuana laws between 1999 and 2010 saw, on average, about 25 percent fewer opiate overdose deaths than states without such laws. What’s more, the effect of a medical marijuana law appeared to grow over time – more lives were saved each additional year after the laws’ implementation, suggesting an effect from more people taking advantage of the programs.
This, of course, is just an observational study. It looks at the correlation between medical marijuana uptake and opiate deaths, but it isn’t able to say that the former definitively caused the decline in the latter. But these findings were soon borne out by other research.
Related stories
- Medical marijuana could help combat opioid epidemic
- Sean Spicer correlated marijuana use to opioid addiction. Medical research is not on his side
- Georgia legislature eyes medical marijuana expansion, craft beer sales and opioid addiction response
- I’ve seen the opioid epidemic as a cop. Living it as a patient has been even worse.
Access to medical marijuana dispensaries is associated with less prescription painkiller abuse, and fewer overdose deaths.
A 2015 working paper published by the National Bureau of Economic Research found that the presence of medical marijuana dispensaries in a state was linked to a 15 to 35 percent decrease in admissions to substance abuse treatment centers, along with a similar decline in overdose deaths.
This study was somewhat more rigorous than the previous paper, drawing on a larger data set that stood up to greater statistical scrutiny. As one of the authors told me at the time, “If this is for real, it means that there are other ways that are less dangerous [than prescription painkillers] for people to deal with chronic pain.”
Medical marijuana is associated with fewer opiate-induced car crashes.
A 2016 Columbia University paper zeroed in on a different facet of the substance abuse problem – auto accidents. The researchers found that after a state passes a medical marijuana law, fewer drivers in those states test positive for opioids after fatal car crashes.
The take-home here is pretty simple: “in states with medical marijuana laws, fewer individuals are using opioids,” the authors conclude.
Painkiller prescriptions fall sharply after medical marijuana laws are introduced.
A novel study conducted last year looked at what happened to Medicare Part D painkiller prescriptions after states passed medical marijuana laws.
It found that the typical physician in a medical marijuana state prescribed 1,826 fewer painkiller doses for Medicare patients in a given year. Why? Some seniors don’t need painkillers if they have access to medical pot (related: seniors and people in late middle age are among the fastest growing marijuana use demographics).
Among chronic pain patients, marijuana use is associated with less opiate use.
A study published last year in the Journal of Pain found chronic pain patients who reported marijuana use were 64 percent less likely to report opiate use, more likely to report good quality of life, and less likely to report negative side effects from their medication.
“This study suggests that many chronic pain patients are essentially substituting medical cannabis for opioids and other medications for chronic pain treatment, and finding the benefit and side effect profile of cannabis to be greater than these other classes of medications,” the authors conclude. “More research is needed to validate this finding.”
“More research is needed.” Researchers universally say they need to do more studies to tease out the nature of the relationships seen in the studies above. In particular, what’s sorely lacking are controlled experiments that allow doctors to treat either chronic pain or opiate dependency with medical marijuana.
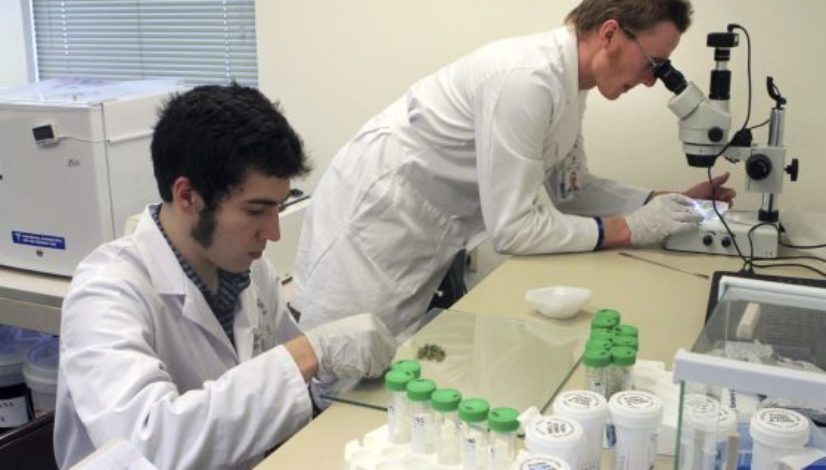
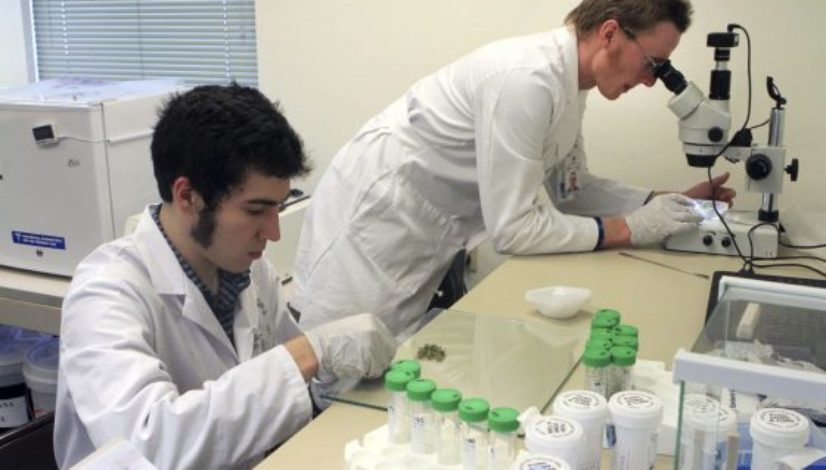
But as of right now that research is incredibly difficult to do because of how marijuana is classified by the federal government. As a Schedule 1 controlled substance, the government has deemed that marijuana has “no medically accepted use.”
Researchers can still work with it, but it requires jumping through an onerous system of legal hoops that can sometimes take years to navigate. It took nearly a decade for one researcher trying to use marijuana to treat PTSD in military veterans to obtain all the approvals necessary.
Those roadblocks have a chilling effect on marijuana research, as outlined in a 2015 Brookings Institution report. Meanwhile, while researchers fight red tape, tens of thousands of opiate users are dying.
The scientific evidence available so far indicates marijuana holds great promise for mitigating the effects of the opiate epidemic. Researchers desperately want to know more, but as long as the Drug Enforcement Administration considers marijuana a Schedule 1 controlled substance, they’ll have a hard time getting more answers.
Topics: Jeff Sessions, opioid epidemic, research